

Understanding Virtual Health
For some health problems, a phone call or video call with a doctor or nurse can save you time and money. This is called virtual care. It may also be called telemedicine or telehealth. Many hospitals and clinics offer virtual care as another way for you to see a doctor.
You will use a computer, phone, or other device to talk to a doctor or nurse. You may have a live video connection. This may be done from a doctor's office so you can talk to a provider who is somewhere else. Or you may be able to connect from your home.
The doctor or nurse can ask you questions. They may be able to check your blood pressure, pulse, and other body functions through special tools connected to your computer. You might also get a virtual physical examination, if you have the right connection (The Future of Virtual Health, n.d.)
Digital health, Telehealth, Telemedicine, Virtual care — What’s the difference?

We think virtual health will be the near-default option for well-being and care in the future of health. But even today, virtual health has shown value in improving well-being and care delivery, along with better patient engagement and experience (The Future of Virtual Health, n.d.)
Virtual Health driving forces

We think virtual health will be the near-default option for well-being and care in the future of health. But even today, virtual health has shown value in improving well-being and care delivery, along with better patient engagement and experience (The Future of Virtual Health, n.d.)
Guiding Principles of Virtual Care
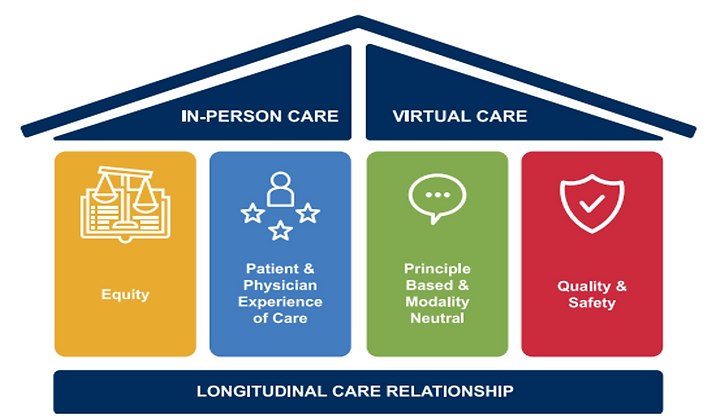
Family physicians are the cornerstone of primary care in BC. As we transition out of the pandemic, it’s time to address the supports and reforms necessary to ensure the stability and sustainability of family medicine within a broader, integrated system of primary care. In order to do so, BC Family Doctors believes that we must hold these four key principles as our guiding ‘truths’ as we move towards a virtual-enabled healthcare system in BC (The Future of Virtual Care - BC Family Doctors, n.d.).
Equity as a Top Guiding Principle of Virtual Care

EQUITY AND ANTI-RACISM We commit to tackling systemic discrimination. We pledge to address the harms that racism inflicts on our patients, our colleagues and ourselves. We commit to confronting inequity in all its forms, from differential access to care to the gender bias in women’s health care delivery and funding (The Future of Virtual Care - BC Family Doctors, n.d.))
What is a Hybrid Model of Healthcare?

A hybrid model of healthcare combines in-person and virtual patient visits to ensure optimal care and it will become a standard feature of the health sector, moving forward. Depending on a patient’s unique clinical requirements, health professionals will always need to have face-to-face appointments available for their patients. However, there are many situations when virtual care that utilises advanced telehealth technology can be used to deliver clinical care to remote patients. The combined use of in-person and virtual visits is called ‘hybrid care’. Hybrid care improves coordinated care across the patient journey by providing health professionals and patients with greater flexibility in how, when, and where they engage. Whether a GP practi[c]es family medicine in a rural clinic, or a medical specialist consults in a busy city practice, hybrid care has an important role to play: From triaging patients and managing chronic conditions, to pre-operative appointments and post-surgery care, a mixture of face-to-face visits and virtual appointments ensures patients receive optimum access to professional care. The important thing is, both clinicians and patients have the choice of whether to meet in-person, or to engage remotely (Carroll, 2022).
Privacy and Confidentiality in Virtual Care
CMPA - Professionalism and ethics | Privacy and Confidentiality | CMPA Good practices (cmpa-acpm.ca)

Patients share sensitive, often intimate information with their doctors. Physicians have a legal, ethical and professional duty to protect patients’ confidentiality and privacy. The legal duty to keep a patient’s personal health information (PHI) confidential originates from the trust relationship between doctors and patients. Privacy legislation reinforces this duty and requires an individual's consent before their PHI can be accessed, collected, used, or disclosed, subject to specified legal exceptions. The duty of privacy and confidentiality applies to every health provider and staff who has access to medical records. Trust in the confidentiality of an encounter and the protection of the information recorded as a result encourages the patient to provide their doctor with all relevant information, enabling the physician to determine the diagnosis and treatment, and reducing the possibility of harm for the patient (Professionalism and Ethics | Privacy and Confidentiality | CMPA Good Practices, n.d.)
How Can Healthcare Professionals Manage the Risks of Virtual Care?

... [A]s our reliance on mobile devices, digital platforms, and online solutions grows, so will our exposure to risk. For many businesses, this may be the first venture into working completely virtual. Infrastructure holes are bound to happen. And even if you do everything in their power to safeguard client information, a third-party could still gain access to information through illegal means ... [t]hat’s why the best practice of all, no matter what you do or who you work with, is insurance (Connection, 2022).
Legal and Practical Considerations for Virtual Health Care in Canada

While we haven’t yet seen a lot of cases in this area, the legal risks are similar to those in the traditional provision of health care, such as medical malpractice, she explained. Technology limitations like poor video quality, inability to pick up on non-verbal cues and lack of physical contact with the patient pose additional challenges. There are also concerns around privacy—particularly access to personal health information—as well as variability and continuity of care, since patients often wind up seeing more than one practitioner (Hodder, 2021)
BCMHSU Virtual Health Services

Virtual health care is today's house call. Care providers can connect directly with people using digital technology. It's a patient-centred approach to care that removes access barriers and is a natural extension of the digital tools many already use (Virtual Health Services, n.d.)
Fraser Health Virtual Care

Since its launch in 2020, Fraser Health Virtual Care has helped more than 198,072 patients, and counting, with their health care needs. Ever wondered where to go when faced with a child's sudden fever or minor injuries like cuts and scrapes? Skip a visit to an urgent and primary care clinic or the emergency room and consider an online Virtual Care visit instead. Virtual Care ensures immediate virtual access to registered nurses, available seven days a week. They can provide non-emergency care for various conditions from the comfort of a person’s home, using any smartphone, tablet or computer. The core mission of Virtual Care is to connect people with the most suitable health resources for their specific needs. “The team assesses patients early on to determine the best care option,” emphasizes Min Naruki-van Velzen, director of operations, Virtual Care. “By doing so, they can direct those who might seek emergency department care to more appropriate services, potentially reducing the emergency department use for lower acuity patients. So, what exactly is Fraser Health Virtual Care? Virtual Care is a secure online health care service that allows patients to remotely connect with registered nurses. With just a few clicks, they can receive health care advice or connect with the appropriate Fraser Health program or service without the need for in-person visits. This helps them save time, eliminates travel hassles and ensures effortless access to health care. Individuals can choose a time that works for their schedule, even during evenings and weekends. This helps ensure health care remains readily accessible beyond regular working hours. To access Virtual Care, patients can simply visit fraserhealth.ca/virtualcare or call 1-800-314-0999 (Fraser Health Virtual Care, n.d.)
